Elevance Health (ELV)·Q4 2025 Earnings Summary
Elevance Health Q4 2025 Earnings: In-Line Quarter, But 2026 Guidance Crushes Stock
January 28, 2026 · by Fintool AI Agent
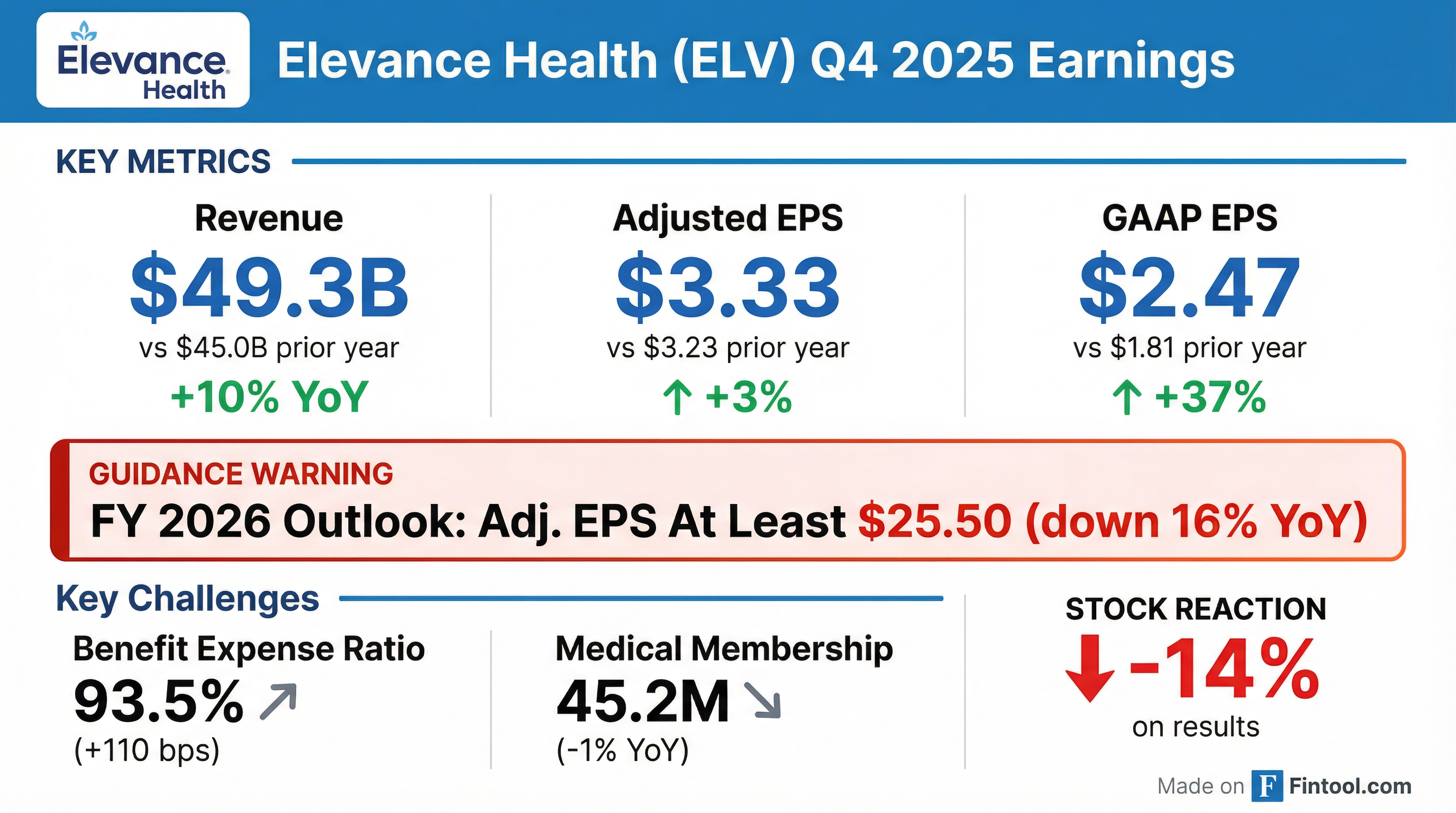
Elevance Health (ELV) delivered Q4 2025 results "in line with our outlook" but shocked investors with FY 2026 guidance implying a 16% adjusted EPS decline . The stock plunged 14% to $322.92 on the news, with afterhours trading pushing shares below $303—down 20% from pre-earnings levels.
The headline numbers looked fine: Q4 operating revenue of $49.3B grew 10% YoY, and adjusted EPS of $3.33 edged up 3% from $3.23 . But elevated medical cost trends, Medicare Advantage membership headwinds, and Medicaid redetermination attrition are converging to create what management characterized as a "recalibration year" for 2026.
CEO Gail Boudreaux framed 2026 as a transition year: "2026 is a year of execution and repositioning, and the outlook we provided today reflects prudent, achievable assumptions grounded in pricing discipline, operational rigor, and targeted investments...As those actions take hold, we expect to return to at least 12% adjusted EPS growth in 2027 off our ending 2026 earnings baseline" .
Did Elevance Health Beat Earnings?
The quarter was largely in-line with management's prior outlook. Revenue growth was driven by higher premium yields in Health Benefits, contributions from acquisitions, and growth in Medicare Advantage membership . However, the benefit expense ratio of 93.5% (+110 bps YoY) reflects "higher medical cost trend primarily in our Affordable Care Act health plans and heightened Medicare Part D seasonality driven by Inflation Reduction Act changes" .
For the full year, operating revenue reached $197.6B (+13% YoY), but adjusted diluted EPS of $30.29 declined 8.3% from $33.04 in FY 2024 .
What Did Management Guide for 2026?
The 2026 outlook is the story. Management issued guidance that implies significant earnings pressure:
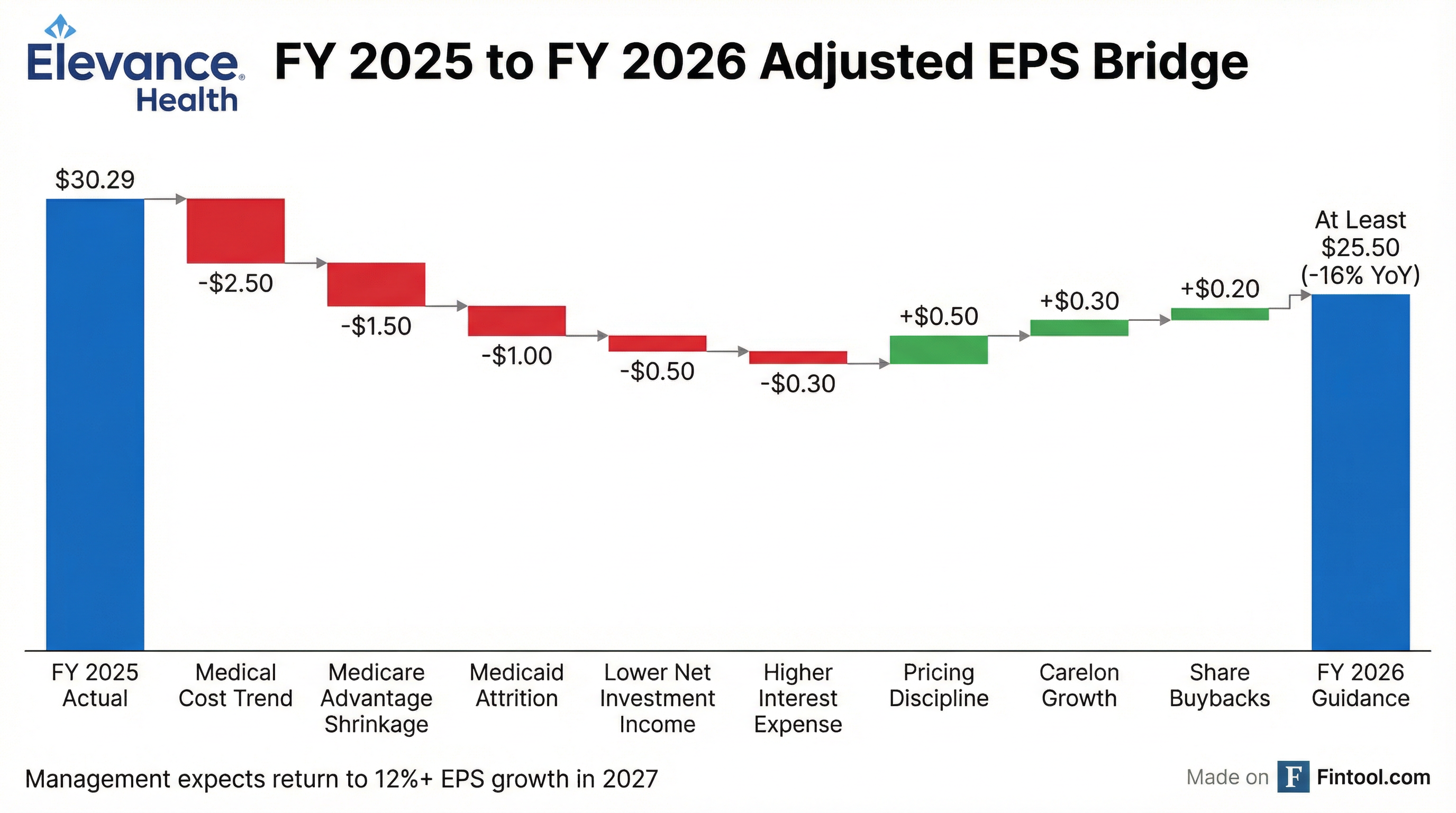
Key drivers of the guidance cut:
- Elevated Medical Cost Trends — The benefit expense ratio is expected to remain elevated at 90.2% , with continued pressure from ACA plan utilization and Medicare cost trends
- Medicare Advantage Membership Decline — Year-end MA enrollment expected to decline in the "high teens %" range, reflecting deliberate portfolio actions
- Medicaid Margin Pressure — Operating margin expected to be approximately -1.75% for 2026, with rates lagging mid-single digit cost trends
- Lower Investment Income — Net investment income guided to $1.875B vs $2.194B actual in FY 2025
- Higher Interest Expense — Projected at $1.53B vs $1.40B in FY 2025
Long-Term Margin Target Revision: Management recalibrated long-term margin expectations: enterprise target now 5%-6%, with Health Benefits, Carelon, and CarelonRx targeting mid-single-digit margins. CEO Boudreaux emphasized: "These updates are intended to provide a clearer, more durable framework for evaluating performance, and they do not change our focus on disciplined execution, durable earnings growth, and strong cash generation" .
Management emphasized this is a "trough year" for repositioning, with the long-term earnings algorithm intact and expectations to "return to at least 12% adjusted EPS growth in 2027" .
How Did the Stock React?
The market reaction was initially severe, then partially reversed:
The initial 14% single-day decline on Jan 27 ranks among Elevance's worst earnings reactions in recent memory. Trading volume of 5.8 million shares was nearly 4x the 20-day average, reflecting institutional repositioning on the guidance cut. However, shares rebounded 4% on Jan 28 as investors digested the "trough year" narrative and 2027 recovery expectations.
The stock has struggled throughout 2025, with shares down from a 52-week high of $458.75 as the managed care sector faced multiple headwinds: elevated medical cost trends, V28 risk model changes, Medicare Advantage star rating pressures, and Medicaid redetermination attrition.
What Changed From Last Quarter?
The Q4 results continued the challenging trends from Q3, but the 2026 guidance represents a meaningful downshift in expectations:
Health Benefits segment posted an adjusted operating loss of $0.2B in Q4, down from a gain of $0.2B in Q4 2024 . Full-year adjusted operating gain of $4.2B declined from $6.3B, a 33% drop .
Carelon remained a bright spot with operating revenue up 27% to $18.7B in Q4, driven by CarelonRx product revenue growth, Carelon Services risk-based solutions expansion, and the CareBridge acquisition . Full-year adjusted operating gain grew 10% to $3.4B .
What Did Management Say About Medicare Advantage?
The Medicare Advantage outlook is perhaps the most concerning element. Management guided year-end 2026 MA enrollment to decline in the "high teens %" range, reflecting deliberate portfolio actions and stability in dual-eligible membership .
Felicia Norwood, President of Government Health Benefits, provided color on the AEP results: "While our outlook for our membership is going to be in the high teens percentage scale reference, and this is below our expectations, we're really pleased at how members reacted to our emphasis on D-SNP, as well as our HMO products" .
Key factors driving the MA membership contraction:
- PPO Product Attrition — "A majority of the attrition occurred in PPO products and in HMO products, in geographies where we didn't offer a comparable alternative"
- Deliberate Exits — "The products and the members that we exited were less aligned with our long-term objectives"
- D-SNP Focus — Company intentionally emphasizing dual-eligible special needs plans
- Margin Improvement — "We're positioned to deliver meaningful Medicare margin improvement to at least 2% in 2026, which is a meaningful step up year-over-year"
Management is implementing "pricing discipline" to restore segment margins, accepting membership attrition in exchange for improved unit economics.
Segment Performance
CarelonRx delivered strong results with quarterly adjusted scripts up 6.8% YoY to 88.5 million and operating margin expanding to 6.2% from 5.3% . Management noted this was their "best growth year ever" with increasing success in large upmarket jumbo accounts .
Pete Haytaian, President of Carelon, explained the long-term margin target adjustment: "We're starting to see a lot more large upmarket jumbo accounts flowing through our business. So that's one factor, and that comes with a different margin profile. In addition, we continue to build out our specialty business...and again, that comes with a bit of a lower margin profile" .
Carelon Services saw revenue surge 47% on the expansion of risk-based solutions, though operating margin compressed as the business scales . External growth remains strong, with Haytaian noting: "If you take out that internal membership headwind, our overall growth would have been on the services side, high teens, low twenties, and on the Rx side, in the low double digit range" .
Capital Allocation & Balance Sheet
The board declared a Q1 2026 dividend of $1.72 per share (+0.6% vs Q4 2025), payable March 25, 2026 . Management has $6.7B of remaining share repurchase authorization .
Investment Pull-Forward: Management pulled forward approximately $0.25 of the ~$1 incremental investments originally planned for 2026 into Q4 2025, using better-than-expected tax favorability. CFO Kaye noted they also "deployed an additional $0.25 towards retention and targeted workforce investments" . For 2026, M&A will take a back seat: "At least in the first half of 2026, you should expect a lower level of M&A activity and a much greater relative emphasis on opportunistic share repurchases" .
Operating cash flow of 0.8x GAAP net income in FY 2025 was below the company's typical 1.0x+ conversion, though management guides improvement to "at least $5.5B" in FY 2026. CFO Kaye explained: "Cash flow in December was negatively impacted by the timing of certain Medicaid-related payments, which were subsequently received in early January" .
Q&A Highlights
The earnings call Q&A session surfaced several key themes:
Medical Cost Trend Outlook (A.J. Rice, UBS)
Q: Are you assuming similar cost trends in 2026 as 2025, or any improvement?
CFO Mark Kaye: "In Medicaid, we expect cost pressure to remain pressured again in 2026, at roughly twice the historical average...That said, after two years of fairly unprecedented trend, we do expect some moderation versus 2025. So you could think about cost trend here moving into that mid-single digit range" .
Key trends by line of business:
- Commercial Large Group — Cost patterns and margins "largely consistent with what we saw in 2025, meaning an elevated but stable trend environment"
- ACA — "Accelerating cost trends, especially as the expiration of the enhanced premium subsidies affects the risk pool"
- Medicare — Higher reported cost trends in 2026, "largely driven by our membership mix, including a greater emphasis on the DSNPs"
Flu Impact (Mark Kaye)
Management flagged a "meaningful uptick in influenza-like activity in December" with "a modest adverse impact on the fourth quarter Benefit Expense Ratio." For Q1 2026, they are "expecting first quarter headwind of about 20 basis points for flu" already embedded in guidance .
Medicaid Rate Outlook (Lance Wilkes, Bernstein)
Q: What's the rate outlook for 2026 and how should we think about it going forward?
Felicia Norwood: "We are contemplating a composite rate increase in 2026 in the mid-single-digit % range, net of certain known Risk Corridor impacts...The final rates that we've received from states for January, and as you know, January represents about a third of our Medicaid premium, those rates were in line with our expectations. But for these states, the rates, while modestly above the historical levels, will still lag trend in 2026" .
2027 Growth Confidence (Josh Raskin, Nephron)
Q: What gives you confidence to confirm the long-term EPS growth target of 12%+, starting in 2027?
CEO Gail Boudreaux: "The key earnings levers are already in motion...Second, our 2026 outlook is intentionally prudent, so as those actions mature, we can capture more operating leverage, and that sets up a clear step-up into 2027. And third...the path isn't predicated on a single assumption. It's built on multiple independent levers and disciplined execution across commercial Medicare, Carelon, and Medicaid" .
Commercial Success: Second Blue Bid
Morgan Kendrick, President of Commercial Health Benefits, highlighted a strong National Accounts season: "We had about 11 bids in the second blue category for 2026, won 9 of them, and the tee up of the actual pipeline for 2027 looks strong and also 2028" .
The Second Blue Bid process allows employers in competing Blue Cross territories to select Anthem-affiliated plans as an alternative carrier, representing a significant growth opportunity.
Risks and Concerns
Several risk factors warrant monitoring:
-
Medical Cost Sustainability — The 93.5% Q4 benefit expense ratio and 90% full-year ratio reflect persistent cost pressures. Management's ability to reprice products to restore margins is critical .
-
Medicare Advantage Execution — The projected 16-20% MA membership decline is aggressive. Execution risk exists around repricing while retaining profitable members .
-
Medicaid Headwinds — Membership expected to decline ~750,000 in 2026 due to ongoing reverification activity. Management expects Medicaid operating margin of approximately -1.75% for 2026, viewing it as a "trough year" .
-
One Big Beautiful Bill Act — New federal legislation introduces eligibility and community engagement requirements that "may cause Medicaid membership to decline, and the acuity of the population may shift over time" .
-
2027 Recovery Path — Management's confidence in returning to 12%+ EPS growth in 2027 depends on successful margin restoration and stable utilization trends .
-
Regulatory Environment — CEO Boudreaux addressed the 2027 MA Advance Notice: "At a high level, the Advance Notice is effectively flat...it just doesn't keep pace with the current medical costs and utilization trends, and that does create real pressure on benefit stability and affordability for seniors" . If funding continues to lag costs, "the levers that we have are benefits, networks, premiums, and exiting geographies" .
Forward Catalysts
- Q1 2026 Earnings — Will provide early read on FY 2026 trajectory and 2026 AEP enrollment
- Medicare Advantage Star Ratings — Fall 2026 release will impact 2027 payment rates
- Investor Day — Potential update on long-term strategic priorities and margin restoration path
- 2027 Guidance — Will be critical test of management's 12%+ EPS growth commitment
Key Takeaways
- Q4 was fine; 2026 is the problem — In-line quarterly results overshadowed by guidance calling for 16% adjusted EPS decline
- Medical costs remain elevated — Benefit expense ratio of 93.5% (+110 bps YoY) reflects persistent utilization pressure, with flu adding 20 bps headwind expected in Q1
- Medicare Advantage reset underway — High-teens % membership decline expected as company reprices for margin sustainability; targeting at least 2% operating margin
- Medicaid trough year — Operating margin of -1.75% expected as rates lag mid-single digit cost trends; federal legislation (One Big Beautiful Bill Act) adds uncertainty
- Carelon remains a bright spot — Best external growth year ever despite affiliated membership headwinds; high teens/low twenties underlying growth in services
- Commercial momentum — Second Blue Bid success (9 of 11 wins) positions national accounts for continued growth
- Management maintaining long-term confidence — Expects return to 12%+ EPS growth in 2027, supported by "multiple independent levers" across all segments
Data sourced from Elevance Health Q4 2025 8-K filing and earnings call transcript dated January 28, 2026